The Problem: Opaque Pricing and Limited Competition
Healthcare in the United States continues to grapple with rising costs and varying quality of care. Unlike other industries that leverage competition and price transparency to boost efficiency, healthcare has struggled to adopt these principles. Integrating competition and transparent pricing could enhance care quality, reduce expenses, and empower patients with better choices. Examples from the U.S. and global healthcare systems underscore the profound impact of these strategies.
The Impact of Opaque Pricing
U.S. healthcare costs is famously unclear and complex. Patients frequently face hidden costs, only learning their expenses post-treatment, which often leads to unexpected financial burdens. Opaque pricing prevents consumers from seeking value and removes pressure on providers to enhance efficiency or quality.
A 2021 study by the RAND Corporation revealed that hospital prices in the U.S. are, on average, 247% higher than Medicare rates (RAND Corporation, 2021, source). A 2024 survey by PwC revealed that 28% of consumers delayed or skipped medical care due to financial constraints, with younger generations, such as Gen Z and millennials, experiencing even greater difficulty.HealthManagement. Without clear pricing, consumers cannot shop for better value, and providers face little pressure to improve efficiency or quality.
The complexity of pricing affects all aspects of the system. For instance, bundled services—such as a hospital stay that includes medications, surgery, and post-operative care—make it difficult for patients to discern how costs are distributed. This opacity further hinders competition because patients cannot easily compare services across providers.
The Role of Competition in Enhancing Quality and Reducing Costs
Competition encourages providers to improve quality and lower prices to attract patients. The generic drug market exemplifies how competition drives down prices while maintaining quality. A 2019 report by the AAM noted that generic drugs saved the U.S. healthcare system $313 billion annually
Case Study: Reference Pricing in California
Reference Pricing: Reference pricing is a healthcare payment model where insurers or payers establish a maximum allowable reimbursement rate for specific medical procedures that is generally tied to regional and national averages or a percentage of Medicare rates. In California, the CalPERS initiative implemented this model for hip and knee replacements, compelling hospitals to compete by offering services at or below the set rate. What were the results?
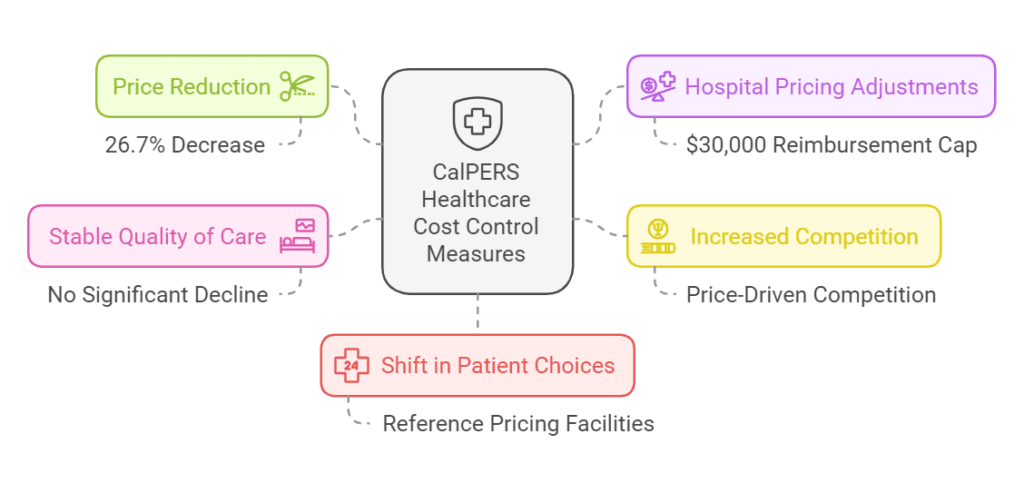
- Price Reduction: Average payments for procedures decreased by 26.7% within CalPERS preferred provider organizations (PPOs).
- Hospital Pricing Adjustments: Higher-priced hospitals lowered their fees to meet the $30,000 reimbursement cap set by CalPERS.
- Increased Competition: Hospitals began competing to offer services at or below the set price, driving overall cost reductions.
- Stable Quality of Care: No significant decline in the quality of treatment despite lower costs.
- Shift in Patient Choices: More patients opted for facilities adhering to reference pricing, reinforcing market-driven cost control.
This approach demonstrates that price caps can incentivize hospitals to operate more efficiently without compromising patient outcomes. Similar models could be expanded to other procedures and states to create broader cost reductions.
The Impact of Price Transparency on Cost and Quality
Transparent pricing allows patients to compare costs, motivating providers to offer competitive rates without compromising quality.
International Examples of Transparency
- Singapore:
- Mandated price disclosure for common procedures.
- Impact: The introduction of the fee benchmarks has been effective in moderating the growth of private surgeon fees, fostering price transparency, instilling discipline in charging, and helping to moderate increases in fees(MOH).
Singapore’s system not only publishes procedure prices but also ranks providers based on quality metrics. This dual transparency empowers patients to make informed decisions while encouraging hospitals to improve their services to remain competitive.
- Australia:
- In response to the need for greater transparency, Zable Health, an Australian company, introduced a digital referral database that displays specialists’ fees, out-of-pocket costs, and wait times.
Zable - Outcome: The platform revealed significant variations in specialist fees, with initial consultations ranging up to $950. By providing detailed cost information, the platform aims to empower patients and encourage specialists to offer more competitive pricing.
- In response to the need for greater transparency, Zable Health, an Australian company, introduced a digital referral database that displays specialists’ fees, out-of-pocket costs, and wait times.
U.S. Examples of Transparency
- Hospital Price Transparency Rule (2021):
- Hospitals required to disclose standard charges.
- Early results indicate improved patient inquiries and competitive pricing (RAND Corporation, 2021, source).
- Employer Innovations:
Walmart’s Centers of Excellence (COE) program stands out as an innovative example of employer-driven transparency and competition. By directly contracting with high-quality hospitals and healthcare providers, Walmart bypasses traditional insurance intermediaries to offer its employees specialized care. Through this program, employees receive certain procedures, such as back surgeries, at little to no out-of-pocket cost, with Walmart covering bundled payments directly negotiated with providers.- Result: Walmart achieved a 50% reduction in back surgery costs, while employees benefited from higher-quality care with fewer complications and readmissions
- By partnering directly with high-performing hospitals, Walmart has demonstrated how employers can influence care quality and costs through strategic transparency and competition.
Consumer Benefits
A 2017 study published in JAMA found that patients who used price transparency tools for outpatient imaging services experienced a 13.9% reduction in payments compared to those who did not use such tools. This suggests that access to pricing information enables patients to make more cost-effective healthcare decisions.
Additionally, price transparency can lead to secondary benefits, such as reducing medical billing errors. When patients and insurers have access to clear pricing information, they are more likely to scrutinize bills, incentivizing providers to ensure accuracy and potentially decreasing billing discrepancies.
Where Price Transparency and Competition Have Fallen Short
Despite successes, some initiatives have struggled to deliver anticipated benefits. Understanding these failures can help design better systems.
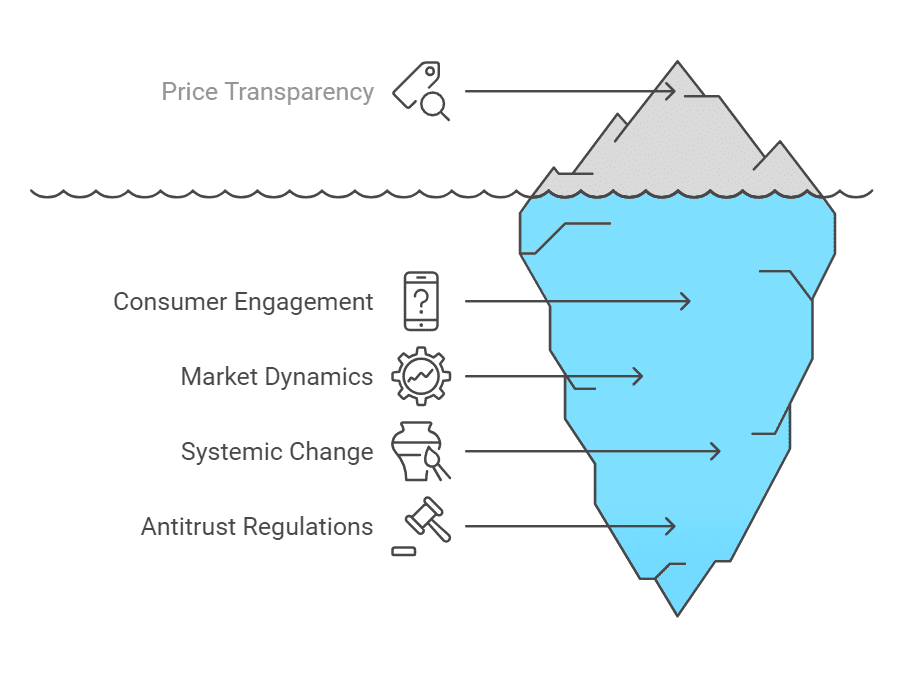
Example: Lack of Consumer Engagement
Even when transparency tools are available, consumers often fail to use them effectively. For instance, a study by JAMA found that only 11% of employees offered price transparency tools utilized them, limiting their impact (JAMA, 2016, source).
Potential Fix: Simplify tools and integrate them with provider platforms to make them more intuitive and accessible. Educational campaigns could also increase awareness and usage.
Example: Market Consolidation
In highly consolidated markets, transparency alone has limited impact. Dominant providers may maintain high prices due to a lack of competition, even with transparent pricing.
Potential Fix: Enforce antitrust regulations to prevent excessive consolidation and foster competition. Additionally, incentivizing new market entrants could create more options for patients.
Policy Recommendations
Strengthen Enforcement
- Increase penalties for non-compliance with price transparency rules. Hospitals failing to meet disclosure standards should face meaningful financial consequences.
Promote Competitive Markets
- Enforce antitrust laws to limit excessive consolidation. Federal and state governments should closely monitor mergers and acquisitions in healthcare.
Expand Consumer Tools
- Develop user-friendly platforms for comparing prices and quality metrics. These tools should be accessible via smartphones and integrated with existing healthcare apps.
Educate Consumers
- Launch public awareness campaigns to help patients utilize transparency tools effectively. Highlighting success stories could motivate broader adoption.
Encourage Value-Based Care
- Shift reimbursement models from fee-for-service to value-based care. This approach aligns provider incentives with patient outcomes, ensuring that cost reductions do not compromise quality.
Conclusion
Competition and price transparency are essential levers for transforming the U.S. healthcare system. By empowering consumers, holding providers accountable, and fostering efficient markets, these strategies can reduce costs and improve quality. Evidence from domestic initiatives and international examples underscores their potential. However, overcoming challenges will require sustained commitment from policymakers, providers, and consumers.
Transparent pricing and healthy competition are not panaceas but are critical components of a broader strategy to create a more equitable and efficient healthcare system. As more stakeholders recognize their value, these principles could drive the systemic change that American healthcare costs urgently needs.







