Efforts to lower healthcare costs, such as reducing Medicare-associated expenses or capping drug prices, are often met with praise. However, these actions can sometimes create unintended ripple effects, such as increased costs for the under-65 market or other medications. This article explores the evidence supporting and contradicting this cost-shifting phenomenon, evaluates its implications, and offers alternative solutions to reduce healthcare expenses without causing unintended economic consequences.
Understanding Cost-Shifting in Healthcare
Cost-shifting occurs when healthcare providers or drug manufacturers compensate for lost revenue in one area by increasing prices in another. For example:
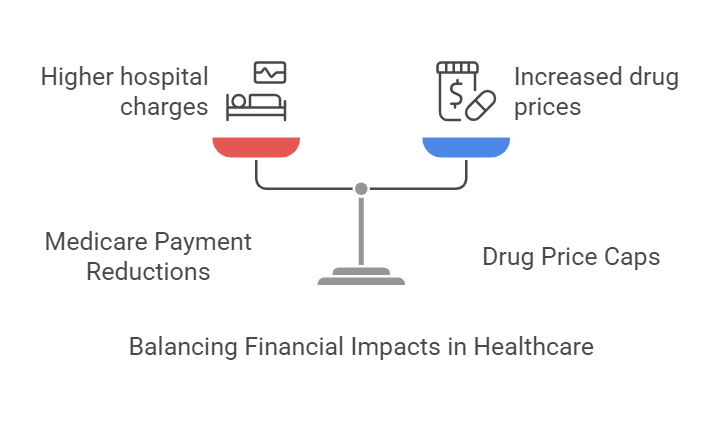
Medicare Payment Reductions
When Medicare reduces reimbursement rates, hospitals may charge higher prices to private insurers to offset losses. This practice helps hospitals maintain financial stability, as the average profit margin for hospitals in the U.S. hovers around 8% according to the American Hospital Association (AHA, 2021). Without such adjustments, hospitals risk operating at a loss, potentially leading to closures or reduced services.
Drug Price Caps
Caps on the cost of certain medications may lead manufacturers to increase prices for other drugs or in other markets. Pharmaceutical companies often cite the need to recover significant research and development costs, which can exceed $2.6 billion per drug on average (Tufts Center for the Study of Drug Development, 2020). Without these price adjustments, companies may struggle to fund new innovations or face financial instability.
Evidence Supporting Cost-Shifting
Hospital Pricing Shifts
- A study published in Health Affairs found that when Medicare reduced payments by 10%, hospitals increased prices for private insurers by 1.6% (Health Affairs, 2019). This 1.6% increase likely did not fully offset the 10% revenue loss from Medicare.
- This practice disproportionately affects individuals with private insurance, as they indirectly subsidize Medicare payment shortfalls.
Drug Pricing Adjustments
- A 2020 study by the National Bureau of Economic Research (NBER) revealed that drug manufacturers often respond to price controls in one market by raising prices in markets with fewer restrictions (NBER, 2020).
- Example: The introduction of price caps in European markets led to a 25% increase in drug prices in unregulated markets like the United States.
Contradicting Evidence
Limited Ability to Shift Costs
- Some experts argue that cost-shifting is overstated. A report from the Medicare Payment Advisory Commission (MedPAC) suggests that competitive market dynamics and insurer negotiations can limit providers’ ability to raise prices for private payers (MedPAC, 2021).
- Example: Insurers in highly competitive regions may resist price increases, forcing providers to find operational efficiencies instead.
Market-Specific Dynamics
- Cost-shifting is less prevalent in markets where alternative funding mechanisms, such as government subsidies or value-based care models, exist to offset revenue losses.
Potential Consequences of Cost-Shifting
Increased Premiums
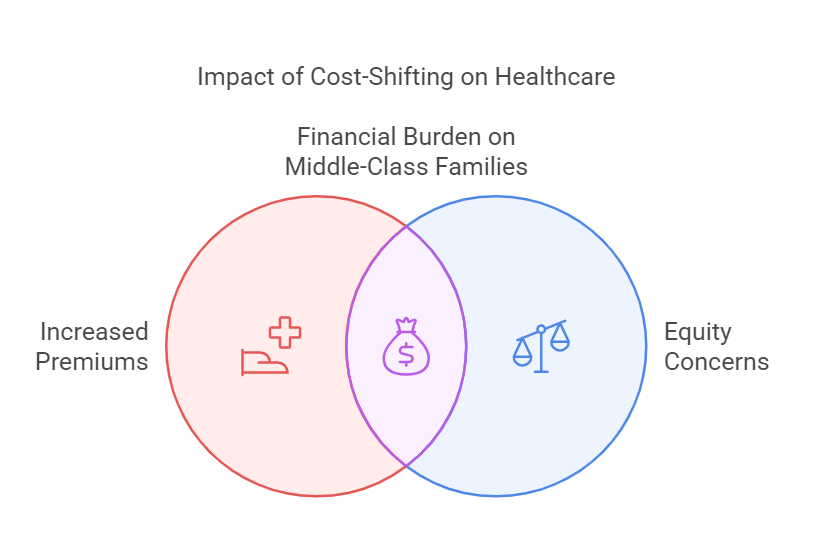
Cost-shifting leads to higher premiums for the under-65 population, eroding affordability for middle-class families.
Innovation Stifling
Higher prices in non-regulated markets may discourage investment in innovative drug development due to reduced affordability and market access.
Equity Concerns
Cost-shifting exacerbates disparities, as those with private insurance bear a disproportionate financial burden compared to beneficiaries of public programs.
Alternative Solutions to Reduce Healthcare Costs Without Shifting Costs
To avoid the pitfalls of cost-shifting, policymakers and stakeholders can consider the following strategies:
1. Promoting Price Transparency
Transparency initiatives, such as requiring hospitals and drug manufacturers to disclose pricing, empower consumers and insurers to make informed decisions.
- Impact: A RAND Corporation study found that transparent pricing could reduce healthcare spending by up to $25 billion annually (RAND, 2021).
2. Expanding Value-Based Care
Shifting from fee-for-service models to value-based care aligns provider incentives with patient outcomes, reducing overall costs.
- Example: The Centers for Medicare & Medicaid Services (CMS) reported a 5% reduction in costs and improved outcomes in its value-based purchasing programs (CMS, 2022).
3. Leveraging Alternative Medication Models
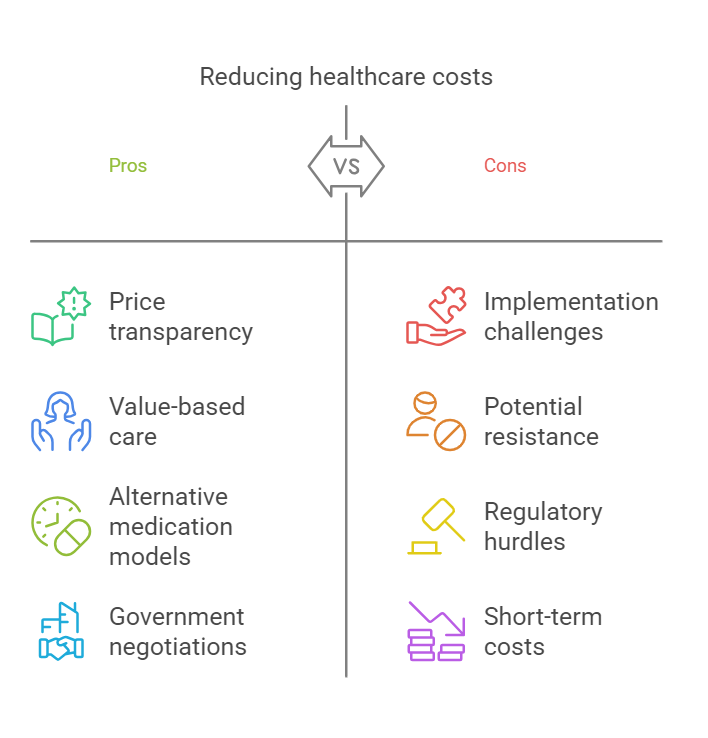
- CostPlusDrugs.com: This platform offers medications at wholesale prices with a small markup, bypassing traditional price-setting mechanisms.
- Employer Programs: Companies like PEO4YOU provide free or heavily discounted generic medications, reducing reliance on costly insurance plans.
- These alternatives can oftentimes reduce medication costs by as much as 80% or more.
4. Government Negotiations and Bulk Purchasing
Allowing Medicare to negotiate drug prices directly with manufacturers can reduce costs without shifting the burden to private payers.
- Example: Countries like Canada and the UK successfully control drug prices through government-negotiated bulk purchasing agreements, achieving lower overall costs.
Challenges to Implementing Alternative Solutions
Resistance from Stakeholders
Insurers, hospitals, and pharmaceutical companies may resist transparency or value-based models due to potential revenue losses.
Regulatory Barriers
Complex state and federal regulations often hinder the adoption of innovative pricing and care delivery models.
Operational Complexity
Transitioning to value-based care or transparent pricing requires significant investment in infrastructure and technology.
Conclusion
Reducing Medicare-associated costs or capping drug prices can inadvertently lead to cost-shifting, increasing financial burdens on other markets or populations. While evidence suggests this phenomenon is real, it is not inevitable. By adopting alternative strategies like price transparency, value-based care, and innovative drug pricing models, the healthcare system can reduce costs sustainably without creating new inequities.
The path forward requires collaboration among policymakers, healthcare providers, and private stakeholders. With the right mix of solutions, the U.S. can achieve a healthcare system that prioritizes affordability, equity, and innovation.







