Access to health insurance is essential for employees and their families to obtain necessary medical care. For businesses, offering health insurance is not just a legal obligation in many cases but also a strategic investment in employee well-being and company growth. But how do companies behave when it comes to providing health insurance, and why is this important?
This article explores the reasons behind corporate decisions on health insurance, the benefits of offering comprehensive coverage, and how intermediaries like PEO4YOU play a vital role in connecting individuals to the best health care options.
In the U.S., the Affordable Care Act (ACA) requires businesses with 50 or more full-time employees to offer health insurance or face penalties. Smaller companies are not legally required to provide coverage, but many choose to do so for competitive reasons.
Reported by the U.S. Department of Labor, businesses that comply with ACA requirements not only avoid penalties but also foster employee trust. Companies that fail to provide insurance risk high turnover rates and legal challenges.
Small firms experience substantial effects from self-funded or level-funded plans under Affordable Care Act (ACA) regulations because these plans provide an alternative method for handling health benefits. Small firms take on the responsibility for their employee health care claims instead of buying standard insurance policies in these health benefit arrangements. Their ability to operate independently enables these small firms to avoid standard insurance premium expenses.
In traditional insurance models companies pay upfront premiums to insurers, but self-funded plans require firms to directly set aside money to handle claims when they happen. Small businesses benefit from the ability to manage their health care costs through self-funding arrangements.
Small firms that operate self-funded plans generally don't need to adhere to certain ACA mandates and state insurance regulations because they opt out of standard insurance policies. The exemption allows employers to create benefits packages that meet their workforce needs more closely while making their employee benefits offerings more appealing.
Small businesses with self-funded or level-funded health plans gain enhanced control over benefits and reduced regulatory burdens from the ACA and state insurance markets.
Health insurance is best regarded as a critical factor in attracting and retaining top talent. In today’s competitive job market, comprehensive benefits packages, including health insurance, are often the deciding factor for job seekers.
According to the 2023 Employer Health Benefits Survey by the Kaiser Family Foundation, 78% of employees prioritize health insurance when evaluating job offers. Companies that provide robust coverage experience higher employee satisfaction and loyalty.
While offering health insurance involves costs, it can also provide significant financial advantages:
Employees at small businesses face financial difficulties when trying to manage complex health insurance systems. Multiple policy options exist which could relieve these financial burdens.
Through examination and application of these policies lawmakers possess the ability to substantially decrease health insurance costs for small firm employees.
The expenses of employer-sponsored health insurance reveal notable differences when examined across small and large businesses within the U.S. The comparison of health insurance costs between small firms and large businesses reveals multiple significant distinctions.
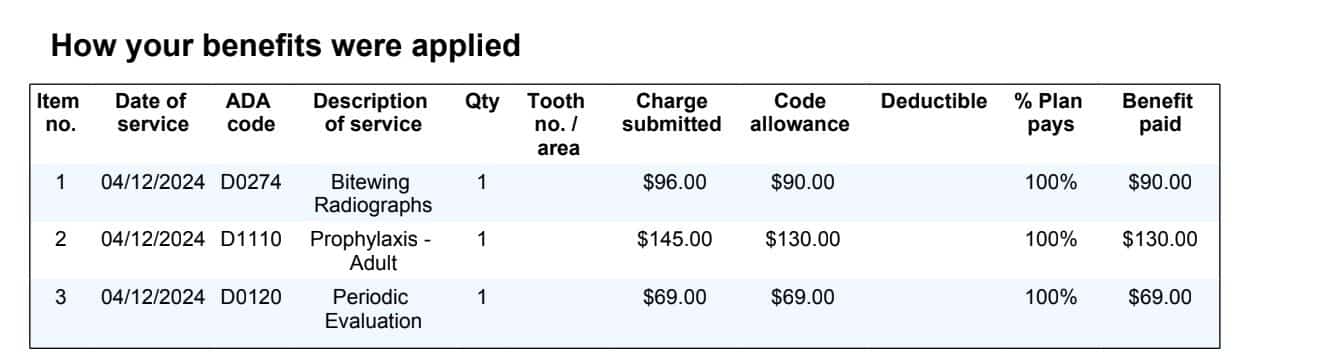
Small Businesses:Staff at small companies usually face higher personal payments towards their health insurance premiums. The typical family premium contribution reached $7,529 during 2023.
Large Businesses: Employees working for large businesses pay lower premiums which averages to $6,796 per family in that year. Although small businesses may present lower total premiums, employees experience more demanding premium costs.
Small Businesses: Employees face higher deductibles which represent the initial payment required before insurance begins to cover most healthcare costs. The average family deductible for health insurance reached $5,074 in 2023.
Large Businesses: Employees working at large businesses benefit from reduced deductibles that average $3,547 for family plans.
Although small business employees face smaller total premium costs, these policies often offer less financial protection. Higher deductible costs mean employees might pay substantially more out-of-pocket before insurance benefits fully kick in. This setup can create a greater financial burden for employees at smaller firms who pay more for plans that cover comparatively less.
In essence, while small businesses may advertise lower total premiums for family coverage, the reality is that their employees often end up shouldering a heavier financial load through both their premium contributions and deductibles compared to those working at larger companies.
Enhanced marketplace premium tax credits have significantly altered the landscape of health insurance, especially for employees of small firms. These tax credits, originally introduced under the American Rescue Plan Act and extended via subsequent legislation, have made health insurance more accessible and affordable. Here’s how they impact small-firm workers:
The continuation of these enhanced tax credits beyond 2025 could be crucial. They not only ensure coverage remains affordable but also help maintain a stable insurance market for small-firm employees.
Many businesses prioritize saving money over offering comprehensive plans. High-deductible health plans (HDHPs) without support like Health Savings Accounts (HSAs) are common, leaving employees with significant out-of-pocket expenses.
Some companies fail to clearly communicate plan details, leading to confusion about benefits and unexpected costs.
Employers often exclude non-full-time employees from health insurance, creating disparities in access to care for vulnerable groups.
Offering basic plans to meet legal requirements without considering employee needs can lead to dissatisfaction and turnover.
High premiums and limited employer contributions make coverage unaffordable for many workers, resulting in lower enrollment rates.
Employees at smaller companies frequently shoulder a greater portion of their health insurance costs compared to those working for larger firms.
In essence, employees at smaller firms endure higher premiums and deductibles while receiving less comprehensive coverage, leading to increased personal financial responsibility.
Excluding mental health services and preventive care undermines employee well-being, leading to long-term costs for both employees and employers.
Healthcare costs in the U.S. have been steadily increasing. Healthcare spending reached $4.3 trillion in 2022 with an expected growth of 5%-6% annually. In 2023, employer-sponsored insurance premiums rose by 7% (CMS,ND)
Multiple elements affect health insurance cost variations between states, particularly for personnel at small businesses. Employees at small businesses across states such as Mississippi, Louisiana and Arkansas typically pay higher percentages of their family coverage insurance premiums than workers at larger companies. Different elements specific to each state create substantial variations in this disparity.
A growing number of small businesses are now choosing to operate with self-funded or level-funded insurance arrangements. Small group employers who choose these plans operate outside Affordable Care Act regulations which may lead to higher insurance premium costs. In markets where self-funded plans enroll healthier employees the remaining risk pool becomes dominated by less-healthy workers which leads to higher coverage costs. Several factors work together to create significant differences in health insurance prices across various states.
Health insurance regulations vary by state, and federal rules like the ACA add layers of complexity. Companies must ensure compliance with coverage mandates, reporting requirements, and nondiscrimination rules.
Employee premium contributions at small firms vary greatly due to state insurance regulations. Employees working at smaller businesses typically pay higher shares of their family coverage premiums than those who work for larger companies.
State-specific rules governing insurance and healthcare markets create disparities in local insurance premiums. Employee contributions towards premiums depend directly on the flexibility or strictness of insurance policies.
These regulations show a great degree of variation which results in visible differences between states. In Mississippi, Louisiana, and Arkansas employees at small businesses must pay more than fifty percent of their family plan insurance premiums. Insurers face higher expenses because of specific regulatory environments and these extra costs get transferred to employees.
State insurance rules form a complicated landscape because they differ from state to state. The amount employees pay toward their premiums changes based on different legislative rules and the diverse conditions found in regional labor markets and different industry sectors.
When it comes to health insurance, small and large firms operate under distinct regulations, impacting both employers and employees differently.
The Affordable Care Act (ACA) holds substantial importance for significant-size employers. Here are the main points to consider:
Small businesses operate under unique regulations and receive special benefits.
The regulations establish significant consumer protections which guarantee equitable and complete health coverage for employees whether they work for small firms or in other market types.
Workforces are increasingly diverse, and one-size-fits-all health plans often fall short. Companies must cater to varying needs, such as:
Small-business owners who learn to handle these challenges can manage health insurance complexities more effectively and stand out as desirable employers in today's job market.
Employees who have access to health insurance are healthier, more engaged, and more productive. Preventive care services, covered under most plans, help employees manage conditions before they become severe.
A study by Health Affairs in 2023 found that companies offering comprehensive health insurance experienced a significant decrease in absenteeism and increase in employee productivity compared to those that did not.
Organizations known for their employee benefits often attract positive attention. Health insurance is a cornerstone of corporate social responsibility (CSR) initiatives, showing that companies prioritize employee welfare.
Health insurance is not just a necessity—it’s a strategic advantage for companies and a lifeline for employees. While businesses face challenges such as rising costs and regulatory complexities, offering health insurance yields significant benefits, from enhanced employee productivity to improved talent retention.By partnering with intermediaries like PEO4YOU, companies and individuals can find the right health insurance options with ease. Whether you’re a business seeking competitive group plans or an individual looking for affordable coverage, PEO4YOU bridges the gap, ensuring that health plans are best tailored to your unique needs.
Recent Posts
Get In Touch— We’re available 24/7
"*" indicates required fields
“We respect your privacy. Your contact information will be used solely for the purpose of responding to your inquiry and will not be shared with third parties.”
Click To Open Modal
Get In Touch— We’re available 24/7
"*" indicates required fields
“We respect your privacy. Your contact information will be used solely for the purpose of responding to your inquiry and will not be shared with third parties.”
Thanks!
We will be in touch soon.
If you're looking to book a consultation now
Affordable health and benefits plans for small businesses, freelancers, and independent contractors.



Copyright © 2026. Peo4you. All rights reserved.